The Hub
Use the links below to log in to access your accreditation portal, register for learning opportunities, and find resources. Stay tuned for an integrated Social Current Hub experience that will centralize access for all the ways you engage with us.
March 24, 2022 @ 2:00 pm – 3:30 pm
An organization’s quality improvement (QI) efforts require continuous nurturing in the form of training, support, and encouragement for staff. During this webinar, participants will gain new tools and strategies for engaging staff and build capacity related to QI.
This session will cover how to form and onboard program staff to the QI process; share practical tools for training and engaging QI teams; and offer strategies for building staff capacity in QI at all levels. Whether you are launching a new QI process or looking to revitalize current efforts, you will take away a variety of new ideas and a toolbox of resources to boost QI at your organization.
About the Performance Excellence SPARK Exchange
This SPARK Exchange (formerly the Performance Excellence APEX) connects professionals who have primary responsibilities for the performance excellence activities of their organizations and provides them with tactical tools, content, shared experience, and advice. The Performance Excellence SPARK Exchange further assists group members in designing effective and evidence-based practices, achieving program goals, increasing client satisfaction, and creating positive client outcomes.
Learn more about promoting a data-driven culture in human services in which all stakeholders are included in the work of performance excellence in the on-demand webinar, Creating a Culture of Performance Excellence.
Learn more about SPARK Exchanges online, and gain access to all of our groups for your staff by purchasing a Social Current Engagement Package.
Takeaways
- How to form and onboard program staff to a quality improvement process
- Participants will gain practical tools and creative ideas for training staff in QI principles
- Participants will feel increased confidence in engaging staff in QI
- Participants will walk out with a toolbox of ideas and strategies for building capacity in QI at their organizations
Who Should Participate
This webinar is relevant for professionals across the human services ecosystem, including those working in the private nonprofit sector, public sector, public policy, or other systems interested in starting or re-energizing their QI systems and how to creatively build capacity and engage staff in the QI processes.
- Quality improvement/data/research staff
- Executives and directors
- Managers and supervisors
- Funders
- Program staff
Presenter

Melissa Curtis
Manager of Performance and Quality Improvement
Lawrence Hall
Related Events
Social Current was pleased to be included at the in-person event to recognize the fifth anniversary of the Family First Prevention Services Act (FFPSA), hosted by the Administration for Children and Families (ACF) at the U.S. Department of Health and Human Services (HHS) in Washington, DC. To mark the occasion, on March 1, 2023, HHS and ACF leadership gathered stakeholders, delivered remarks, and brought together panels of legislators, national experts, and state and tribal leaders. The event featured videos from families with lived expertise in the child welfare system. The conversations reflected a rich understanding of why the legislation was created, what it has accomplished, its challenges, and where we go from here to better support families. The recording for this event is available here.
Five years ago, FFPSA was enacted to enhance upstream and supportive services for families to help children remain safely at home with their caregivers, reduce the unnecessary use of congregate care, and build the capacity of communities to support children and families. At the anniversary event, Social Current observed five takeaways that will help to shape future opportunities to support thriving families and communities.
- Create community pathways to family success outside of child welfare. All families need help sometimes, and we must create pathways for families to receive that help from trusted community-based organizations. Child and family well-being is a shared responsibility across communities, as we all benefit from strengthening families. This responsibility includes child protection but is not limited to it, as it extends to all systems that help to bolster child and family well-being. More and more public systems are recognizing that families are best served in the community. These community pathways will require systems change that normalizes and de-stigmatizes help-seeking behaviors.
- Reduce child welfare’s footprint. As these community pathways are established, child welfare can safely reduce its footprint and effectively serve a smaller population of families. Shifting more resources toward upstream prevention in the community, rather than reacting by the child welfare system, does not mean that we give up our responsibility to keep children safe. Shifting our focus to support families before they are known to child welfare will ultimately mean that fewer children require protection because their families are better supported, safe, and healthy.
- Bring Medicaid and SAMHSA to the table. FFPSA authorized new optional title IV–E funding for time-limited prevention services for mental health, substance use disorders, and in-home parent skill-based programs for children or youth who are candidates for foster care, pregnant or parenting youth in foster care, and the parents or kin caregivers of those children and youth. To move further upstream and support more families outside of the child welfare system, Medicaid can be utilized and accessed for services that can reduce the involvement of child welfare. Medicaid is the single largest payer for mental health services in the United States and is increasingly playing a larger role in the reimbursement of substance use disorder services. This collaboration can be informed by the science generated through the Substance Abuse and Mental Health Service Administration (SAMHSA), demonstrating that addressing behavioral health keeps families strong and together.
- Build the evidence base for cultural adaptation of programs. There is a lack of research models that build the evidence base for cultural adaptation of programs and services, coupled with an awareness that there is disparity across child welfare systems that too often results in more children of color coming to the attention of child welfare. These research models need to be community-engaged and community-designed. The Title IV-E Prevention Services Clearinghouse should prioritize populations and problems that are underserved by the current array of programs. This should encompass communities of color, including Tribal communities. It should also include programs that address domestic violence, economic supports to reduce poverty, and peer/parent mentoring programs.
- See all ACF and other family-support programs as preventative. Our goal should be to invest prevention dollars, including those spent on concrete and economic supports, in more children than the number of children we are removing from their homes and families. To accomplish this, we need to see all family-support programs sponsored by ACF and others as preventative. The human and social services sector is at the forefront of an evolutionary change, one that aims to realign social services to be more preventative with greater upstream resources that focus more directly on addressing the social determinants of health (SDoH) to achieve better outcomes. The potential to improve health outcomes and more fully address SDoH through a public health and a system of care approach with greater investments in human services could transform a range of systems, including health, education, welfare, and criminal justice systems and ultimately result in greater well-being for all families.
Achieving these reforms will require a tremendous shift in resources, both at the federal funding level to redirect funding to more front-end resources, through policies that adapt to a more preventative approach, and in the way that place-based services are delivered by community-based organizations. Passage of FFPSA is a first step in that journey for child welfare. Too many of our social systems were structured to respond only after harm occurs – by realigning our nation’s social service delivery systems and reimagining the power and impact of the social sector, we can deliver on the promise of equitable access to health and well-being for all people.
COA Accreditation, a service of Social Current, is proposing enhancements to its standards that will be released in early 2023.
The Residential Treatment (RTX) standards have been revised to better address important topics in the field, including resident voice and choice, family involvement, trauma-informed care, strategies for reducing the use of restrictive interventions, and how to help residents develop the skills to manage challenges and live successfully at home and in the community.
These recommended updates are now open for review and comment from the field. Download and review the proposed standards. The deadline to make comments is Jan. 11, 2023.
COA Accreditation has also proposed equity, diversity, and inclusion enhancements to its standards to better promote the delivery of equitable services for all people through physically and psychologically safe, welcoming, and trauma-informed environments. Submit feedback on these revisions by Jan. 3, 2023.
These proposed updates reflect an in-depth review and synthesis of prominent published research and professional literature as well as collaboration with a diverse group of subject matter experts from this field. The field comment period is a critical step in our process because it ensures our standards are field informed by including input from provider organizations in the development process.
This critical pairing of research and practice ensures that the COA Accreditation standards remain rigorous, practical, and reflective of current trends and evolving practices and continue to promote improved outcomes for individuals, families, and communities.
We are excited to announce that our COA Measures benchmarking reports are now available for our accredited private and Canadian organizations. COA Measures is the first of its kind human services benchmarking program grounded in years of research.
We began this journey in 2016 with COA’s 2020 strategic planning process. We talked with and surveyed our network regarding their reasons for seeking COA accreditation and how we could provide even more value to their experience. One theme which was raised over and over was the need for data.
This result is the product of years’ worth of work including research, pilots, surveys, and focus groups, that we couldn’t have accomplished without the incredible network of organizations that are part of our accreditation family. The findings cover a wide array of measures of organizational health and sustainability, including finances, workforce, governance, and many more. Accredited private and Canadian organizations can access their benchmarking report via their MyCOA portal.
Thank you to the hundreds of participants in our first ever endeavor, we couldn’t have done this without the generosity and time of our partners. You can learn more about COA Measures here.
June 15, 2023 @ 2:00 pm – 3:00 pm
For anyone working within the human services ecosystem and wanting to develop better logic models, this webinar is here with expert guidance. This webinar will help participants:
- Know which logic model type to use when monitoring the delivery of services to ensure that they are consistent with best practice principles
- Overcome the challenges of modelling complex interventions
We will outline key considerations and provide practical strategies that can help those engaged in performance and quality improvement (PQI) work to identify and mitigate some limitations of logic models. This webinar aims to increase confidence in creating and using logic models for programs/service delivery. The presenter will expand on how a basic logic model can be used in:
- Effective program evaluation
- Collecting, analyzing, and providing data/results to share with stakeholders
- Learning to continually improve programs
The presenter also will take participants through the pitfalls associated with creating a logic model, provide examples of logic models for social and human service-related programs, and show how to expand the logic models’ use in identifying outcomes and collecting and analyzing data that allow for clear results and/or continuous improvement of services. Exercises and examples that focus on the development of a simple service/program logic model to a more complex organizational logic model, including practical examples and a template for developing a logic model.
Takeaways
- The differences between outcomes and outputs using real examples and best practices
- How to use your logic model to help inform your performance and quality improvement initiatives
- Approaches for assessing logic models
- How to revise logic models for increased outcomes
Who Should Participate
- Executive and senior leaders
- Performance and quality improvement professionals
- Leaders in program design and innovation
- Research and evaluation leaders
- Grants management professionals
- Program/department directors and managers
Presenter

Shannon Wichlacz, PhD
Senior Evaluation Associate
CCNY Inc.
Related Events
When it comes to serving communities and responding to individuals in crisis, law enforcement agencies and human service systems each play a role in maintaining the safety and stability of their communities. Substance use, child welfare, intimate partner violence, suicide, juvenile justice, mass violence — these are not only some of the most prominent societal challenges we face today, but also circumstances where both police officers and human service professionals are on the front lines.
The roles of law enforcement and human service agencies therefore consistently overlap. In communities and environments where needs are intensified and resources limited, this overlap comes into sharper focus. When behavioral healthcare is inaccessible, or social service systems are overburdened, communities often turn to law enforcement to fill in the gaps — sometimes leading to serious negative outcomes that can inflict trauma, injury, or death:
- Foster youth arrested and handcuffed for running away
- Mental illness played a role in 25% of fatal police shootings in 2017
- Misunderstanding disability leads to police violence
Such incidents are not only harmful to the individuals involved, but can also irrevocably damage a community’s trust in its police force and social support systems. These trends are a clear indicator that communication and partnerships between law enforcement agencies and human service providers need to be examined and strengthened.
Collaborative approaches to crisis intervention
The relationship between behavioral health and policing cannot be overstated; according to the National Alliance on Mental Illness, individuals in mental health crisis are far more likely to be confronted by police than to receive medical attention. More than 90% of patrol officers encounter individuals in crisis, with an average of 6 encounters per officer per month, but officers are often unprepared to meet the unique challenges of de-escalating a person with a disability or mental illness in crisis. A traditional law enforcement approach — “command and control,” — designed for crime intervention is likely to elicit fear and disorientation in individuals with disabilities or who are in emotional distress. Such approaches pose a significant risk of triggering a trauma response and escalating the dangerous behavior, increasing the likelihood for excessive force to be deployed.
In response to these challenges, law enforcement agencies have increasingly recognized the value of diversifying capacity and expanding officers’ skill sets in order to increase safety and efficacy in crisis response. In addition to ramping up efforts to educate officers on trauma, mental illness, and disability, and expanding training on de-escalation and crisis intervention techniques, many departments are adopting innovative new models to partner with behavioral health and human service professionals in police work.
Crisis Intervention Teams are one popular model in use in 2,700 communities across the country. The core components include recruiting, selecting, and training officers to serve as designated responders to mental health crises, and establishing relationships with a designated mental health receiving facility and other resources in the community to facilitate immediate emergency entry into the mental health system and reduce barriers to care. Officers receive 40 hours of intensive training on common disorders, developmental disability, and crisis de-escalation skills. Key to the success of this model are: ensuring adequate staffing to maintain continuous CIT coverage, equipping emergency dispatchers with the skills needed to identify when a CIT response is appropriate, and designing and delivering training curricula with the collective input of law enforcement, behavioral health specialists, and advocates. Evaluation of the CIT model indicates that it yields positive results, reducing officer injuries as well as the need for more intensive and costly law enforcement responses as well as increased referrals to emergency health care and accessibility of mental health services.
Co-responder programs are another partnership strategy with growing interest. Los Angeles, Omaha, Mesa, Arizona, and Huntington, West Virginia are among the jurisdictions that are adopting or expanding programs in 2019 to embed therapists, social workers, or addiction counselors into police departments. There is no standardized model, and program scope varies widely from place to place: some departments hire behavioral health specialists directly while others coordinate part-time or rotating coverage from a local provider; some target suicide and others substance use; they may be first on the scene or “secondary responders”; responsibilities can range from emergency response, community patrol, or even follow-up and case management. Although the programs are incredibly diverse, the rapid rate of adoption points to a culture shift in law enforcement: an emerging understanding of the agency’s role in responding to complex issues facing their communities, willingness and recognition of the value of working closely with human service professionals, and an investment towards diverting individuals in crisis away from the criminal justice system.
Establishing boundaries
Responding to individuals in crisis in the community is not the only circumstance where law enforcement and human services intersect. Although the integration of social workers and therapists into the world of community policing is a growing trend, for many human service providers — especially resource-starved ones — engaging police departments for assistance is standard operating procedure that may come with unintended consequences.
In a May 2019 lawsuit filed against the Administration for Children’s Services, the New York state appellate court ruled that family courts do not have the authority to issue warrants for foster youth who have run away from their placements — a longstanding practice. In 2017, the child welfare agency was granted 69 arrest warrants for children in their care; that was after guidelines for seeking warrants were tightened in 2015, when the number of arrest warrants issued was up to 125. In a majority of these cases, police officers deployed to retrieve missing youth end up putting them in handcuffs and in jail cells, regardless of safety risk.
Runaway behavior in foster care can often be attributed to trauma — children leave their foster care placements to be with the family members from whom they’ve been separated or other loved ones, or due to conflict with their foster parents. Being apprehended and even restrained by police officers and forcibly returned to settings where they may not feel safe exponentially compounds that trauma. The already fragile (or absent) trust in the child welfare agency may be eroded, often irrevocably, and the agency’s motivation may be perceived as punitive vs. protective.
In congregate care, the intensive needs and challenging behaviors of residents can often overwhelm the capacity of personnel and for many residential facilities, a common response to harmful or disruptive behavior, or unauthorized leave, is to summon police officers. In some communities, police departments report responding to struggling facilities multiple times a day. As with crises that take place in the community, the consequences of calling the police can be significant if the appropriate skills and protocols are not in place. And for organizations, chronic reliance on police intervention poses additional risks: therapeutic setbacks to service recipients involved, damaged staff morale, and diminished perception in the eyes of the host community and collaborating providers.
In 2015, California passed legislation aimed at reducing the frequency of law enforcement intervention in group homes and other residential facilities for children and youth. But policy or regulation is unlikely to be effective if the underlying causes are sidestepped. Experts argue that frequent calls to law enforcement are an indicator of deeper issues: inadequate staffing, insufficient training, ineffective programming, or a need to reassess admission/screening criteria. The continuum of challenges endemic to social services — underfunding, understaffing, burnout, turnover — hamper providers’ ability to meet the needs of their service population and maintain a safe and stable therapeutic environment.
If police intervention is unavoidable, then effective collaboration and proper training is critical. Providers and police departments must ensure that responding officers are familiar with the characteristics and needs of the service population and learn the skills necessary to safely de-escalate, retrieve, restrain a service recipient utilizing the least restrictive response to maintain safety. Recommendations from advocates include:
- Jointly evaluating policies and protocols to emergency response
- Creating Memoranda of Understanding between police departments and providers to better define roles and expectations around interventions, and ensure that responding officers are given relevant details about the residents in crisis
- Better data collection and analysis on the frequency and nature of law enforcement intervention in treatment settings
Children’s Village, a COA-accredited provider in New York, has called upon city leaders to form a Runaway Youth Taskforce to bring together law enforcement and social services in developing a new model for preventing and responding to runaway youth.
Meeting the mental health needs of police officers
A recent cluster of officer deaths by suicide has shed a harsh light on the challenges of addressing the mental health needs of the law enforcement community. Officers are at increased risk of PTSD, depression, anxiety, substance use, and suicide due to constant threat of violence or actual violence and exposure to death and trauma, in addition to chronic work stressors such as sleep deprivation and fatigue. Although repeatedly acknowledged by law enforcement agencies and police union leadership, the mental wellness needs of police officers are still persistently unaddressed. The culture of law enforcement has often been cited as a major barrier to care, with officers reporting fear of perception of weakness, alienation from fellow officers, and other potential professional repercussions as a result of seeking out needed services and supports.
Ignoring the mental health of police officers puts communities at risk. Studies have linked PTSD with impaired decision making ability — a critical implication for police officers in potentially life-threatening situations, and the potential for excessive or deadly force. These incidents not only increase the risk of injury or fatality of those involved, but also negatively impact the relationship between the community and law enforcement.
The human services field may be uniquely positioned to make a positive impact in this area. Professional staff in the social services and behavioral health field share many of the same work stressors as police officers — excessive caseloads, exposure to traumatic events, vulnerability in the community or service environment — and the impact of secondary or vicarious trauma has become a prominent area of research and advocacy in the human services field. Providers can bring significant knowledge to the table for law enforcement agencies about identifying and mitigating the effects of PTSD and secondary trauma, appropriate resources for treatment and support, and strategies for bolstering officers’ resilience.
Increasing the presence of behavioral health professionals in law enforcement settings can provide multiple benefits — not only by distributing or diverting the “social work” attributes of community policing, but also by providing an avenue for officers to seek support and referral to available services. Law enforcement leaders might also consider whether services provided outside of the auspices of the law enforcement agency might be more accessible to officers, potentially reinforcing confidentiality of services and softening the impact of stigma. Service providers can also assess opportunities to expand or tailor their service array in a way that focuses on the unmet needs of this population or supports their families. Research suggests that cultural competency — awareness of and responsiveness to the cultural and professional idiosyncrasies of police work — is pivotal to the accessibility and efficacy of psychological interventions targeted at police officers, and may be enhanced through peer-driven program design.
To protect and serve — and partner
Communities today are recognizing that the most pervasive social and public health challenges they are confronted with cannot be overcome without constructive collaboration between the social service, behavioral health, and criminal justice systems. Successful collaboration hinges, however, on meaningful assessment of areas of strength and need, clearly delineated roles and responsibilities, and a shared commitment to invest in the most effective solutions. Many agencies are developing or pursuing creative strategies to build partnerships between providers and police officers, with the understanding that joining forces is imperative to forming a greater understanding and capacity to meet the needs of their shared community, strengthening public trust and improving outcomes across all systems.
We’d love to hear from any organizations with experience in human services – law enforcement collaboration. Please share any promising practices or lessons learned in the comments below.
Learn more or get involved
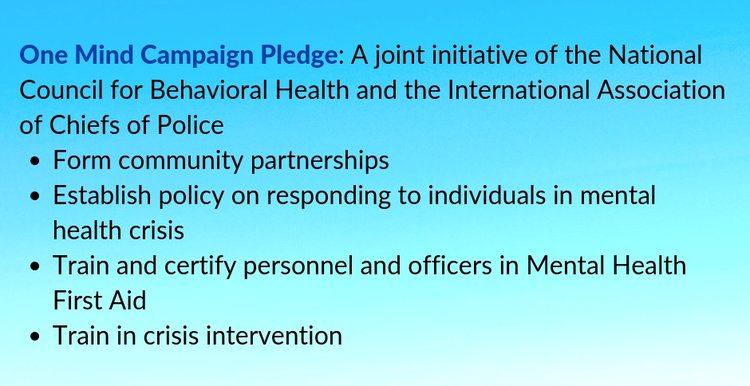
- International Association of Chiefs of Police: One Mind Campaign
- Vera Institute of Justice: Serving Safely initiative
- National Alliance on Mental Illness: Resources for law enforcement officers
Late last week, various federal agencies released more details about new vaccine mandates. The U.S. Department of Labor’s Occupational Safety and Health Administration (OSHA) issued a new federal rule last week mandating COVID-19 vaccinations or at least weekly testing for workers at U.S. companies with 100 or more employees. The OSHA rules are a key part of President Biden’s push to use employer mandates to increase vaccination rates. OSHA is holding webinars to detail these new rules this Tuesday and next Monday. The administration also released a new rule through the Centers for Medicare and Medicaid Services (CMS) that requires workers at health care facilities participating in Medicare or Medicaid to be fully vaccinated by Jan. 4, however, most community-based organizations are excluded from the definition of a “covered entity.” This FAQ from CMS provides more details. This summary of the OSHA rule from the National Council of Nonprofits is a helpful guide to the regulations. For more details, check out our article brief below.
Meanwhile, Congress continues negotiations around the Build Back Better bill. On Friday night, the House passed the physical infrastructure bill and conducted a procedural vote to pass the Build Back Better Act no later than the week of Nov. 15, putting pressure on the Senate to speed up negotiations. Several weeks ago, President Biden released a new framework for the social spending and climate bill based on negotiations. However, he is still seeking the support of Senator Joe Manchin (D-W.V.) to move forward. That version of the bill removed a new paid leave program. However, progressives have negotiated the paid leave provisions back into the bill, creating additional challenges for Manchin to get on board. Independent Sector recently released a helpful summary of current provisions in the bill, which are subject to change as negotiations continue. Some highlights include a one-year extension of the new Child Tax Credit provision from the American Rescue Plan; $300 million for broadband affordability and access; $20 billion for workforce development programs; $150 billion for affordable housing; $100 billion to support child care costs, universal preschool, and more. Congressional leaders seem hopeful that they will pass a bill by Thanksgiving at the very latest.
New Toolkits for Building Your Advocacy Muscle
Social Current offers two newly updated advocacy toolkits, one with general public policy and advocacy how-tos and another with tips for media relations and social media to support advocacy. Inside, you’ll find sections on creating impact stories, engaging with legislators, developing media relations, hosting special events, and conducting social media outreach. They also contain brand new sections on virtual advocacy, constituent engagement and coalition building. Read about how COVID-19 has changed the rules for meeting with legislators and download the toolkits from the Policy Action Center.
New Vaccine Rules for Employers
Late last week, various federal agencies released more details about new vaccine mandates. The U.S. Department of Labor’s Occupational Safety and Health Administration (OSHA) issued a new federal rule mandating COVID-19 vaccinations or at least weekly testing for workers at U.S. companies with 100 or more employees. The OSHA rules are a key part of President Biden’s push to use employer mandates to increase vaccination rates. The first compliance deadline for employers—providing time off for workers to get vaccinated and ensuring those who aren’t vaccinated are wearing masks, is Dec. 5. Workers must be fully vaccinated by Jan. 4 or submit to testing requirements. Some exceptions apply for the vaccine, but otherwise will still require testing and masks. The number of employees is based on all employees (part and full-time combined). Employees working remotely or outdoors are counted for employer coverage purposes, but they may not necessarily be required to comply with the requirements if they don’t come into contact with clients or coworkers. Employers may require employees to pay for the cost of testing, except where other legal or collective bargaining obligations require otherwise. Employers not in compliance could face a fine of up to $13,653 for each violation. A willful violation is an employer deliberately disregarding the mandate, which could result in a fine as high as $136,532. For states with their own standards, implementation could be delayed as governments decide whether to accept the standard as written, modify it, or draft equivalent or more protective rules. Each state has 30 days to implement a standard.
This summary from the National Council of Nonprofits is a helpful guide to the regulations. Additional information from OSHA is also available.
The administration also released a new rule through the Centers for Medicare and Medicaid Services (CMS) that requires workers at health care facilities participating in Medicare or Medicaid to be fully vaccinated by Jan. 4. CMS is requiring that workers at health care facilities participating in Medicare or Medicaid have necessary shots and be fully vaccinated by Jan. 4. It covers approximately 76,000 health care facilities and more than 17 million health care workers. It applies to employees regardless of whether their positions are clinical or non-clinical, essentially any employee, student, trainee, or volunteer who works at a covered facility. It also covers individuals who provide treatment and other services for the covered facility under contract or other arrangements. Covered facility types include hospitals, ambulatory surgery centers, home health agencies, psychiatric residential treatment facilities, rural health clinics, federally qualified health centers, and long-term care facilities. However, it does provide an exemption for certain home- and community-based services.
Several state attorneys general are planning to sue the federal government to block the initiative.
New Ratings in the Family First Prevention Services Clearinghouse
The Title IV-E Family First Prevention Services Clearinghouse recently announced ratings for 13 new programs. One was found to be “well-supported” by research, two were found to be “supported,” three were found to be “promising,” and the rest didn’t meet criteria to be rated. A new comparison between ratings from the IV-E federal Prevention Services Clearinghouse and the California Evidence-Based Clearinghouse is now available.
This brings the total number of programs meeting criteria in the clearinghouse to:
- Mental Health: 6 “well-supported,” 8 “supported,” and 12 “promising”
- Substance Use: 4 “well-supported,” 3 “supported,” and 3 “promising”
- In-Home Parent Skill-Based: 7 “well-supported,” 7 “supported,” and 3 “promising”
- Kinship Navigator: 1 “promising” and 0 “well-supported” or “supported”
New ratings are as follows:
- Aggression Replacement Training® – Promising
- Child-Parent Psychotherapy (Re-review) – Promising
- Circle of Security – Intensive™ – Does not currently meet criteria
- Circle of Security – Parenting™ – Does not currently meet criteria
- Familias Unidas – Well-supported
- Familias Unidas – eHealth – Does not currently meet criteria
- Family Centered Treatment (Re-Review) – Supported
- Helping Women Recover + Beyond Trauma – Does not currently meet criteria
- Ohio’s Kinship Supports Intervention/ProtectOHIO (Re-review) – Promising
- Parenting Wisely – Teen Edition – Does not currently meet criteria
- Parenting Wisely – Young Child Edition – Does not currently meet criteria
- Parenting with Love and Limits® – Supported
- Safe Environment for Every Kid (SEEK™) – Does not currently meet criteria
Source: Child Welfare & Mental Health Coalition
Centers for Medicare and Medicaid Services Publish New Q&A on QRTPs and the IMD Exclusion
The Centers for Medicare & Medicaid Services (CMS) published a Q&A guide to inform states that they can seek to modify the terms of an existing Medicaid section 1115 demonstration opportunity to allow Title IV-E beneficiaries to receive coverage in a Qualified Residential Treatment Program (QRTP) that is an Institute for Mental Disorder (IMD) for longer than that demonstration model currently allows. States with an existing, approved severe mental illness/severe emotional disturbance (SMI/SED) 1115 demonstration would need to submit an amendment to take advantage of this opportunity. For those states that do not currently have the demonstration, approval of new demonstrations will depend on the details of state applications submitted and whether they can meet the current requirements of the SMI/SED 1115 demonstration. As a condition of approval, states will be required to provide CMS with a plan, including key milestones and timeframes, for transitioning children out of QRTPs that are IMDs.
This Q&A clarifies that placement in a QRTP that is an IMD does not impact Medicaid eligibility. It details that the IMD exclusion only prohibits states from receiving federal reimbursement for services delivered. It does not affect a child’s eligibility for Medicaid.
Source: Child Welfare and Mental Health Coalition
Congressional Research Service Releases Report on Chafee Funds
The Congressional Research Service released a new report on the status of funding for youth who have or are about to age out of care. Major provisions in the John H. Chafee Foster Care Program for Successful Transition to Adulthood Act expired Sept. 30, 2021, the end of the 2021 fiscal year. These funds included Education and Training vouchers, which allow states to assist youth with room and board payments and postsecondary school or training until age 27. The report states that a large majority of states pulled down less than 50% of Chafee funds available to them last year, meaning that critical funds are in limbo. Reps. Danny Davis (D-Ill.) and Jackie Walorski (R-Ind.) co-sponsored H.R. 5661, which passed the House of Representatives in October, extending funding flexibilities for another year; however, the Senate has yet to take up the companion bill (S. 3078).
Social Determinants of Health Caucus Holds First Congressional Briefing
The Congressional Social Determinants of Health Caucus hosted its first briefing focusing on transportation as a critical component of population health and well-being. Reps. Cheri Bustos (D-Ill.), Markwayne Mullin (R-Okla.), G. K. Butterfield (D-N.C.) and Salud Carbajal (D-Calif.), members of the Social Determinants of Health Caucus, highlighted transportation barriers as a key challenge to individuals and families having access to pharmacies, hospitals, and other health care centers. Especially in rural areas, lack of transportation options severely impacts one’s ability not only to receive care, but also to access employment, education and other social services that are central to well-being. In July, the caucus was formed to raise awareness about health disparities and come up with solutions that increase long-term health and well-being.
May 23, 2022 @ 1:00 pm – 4:00 pm
Three CEU Credits (Social Work): Approved by the NASW-Michigan Social Work Continuing Education Collaborative. Please check with your local accrediting body for reciprocity.
This training introduces participants to a social identity framework focused on sexual orientation, gender identity, and gender expression (SOGIE). In addition to learning about SOGIE in the context of social identities, participants will also review best practices to enhance interpersonal and professional relationships with clients and peers who identify as LGBTQ+ or have diverse/expansive SOGIE.
This training series is interactive, and participants are asked to be on camera and able to interact with other participants through video, audio, and chat periodically. While this is an expectation of the training, we understand that there can be barriers to this type of involvement. Reach out to the trainers ahead of time at for more information or accommodations.
Objectives
- Why we are discussing SOGIE (statistics, evidence-based practices, personal narratives)
- Introduction to social identity framework
- The difference between assigned sex, gender identity, gender expression and sexual orientation
Who Should Participate
- Professionals who work with children, youth, young adults, and/or families who are at a beginner level of knowledge on sexual orientation, gender identity, and expression
- Participants can be individuals who directly with others or be involved in supervision, management, and leadership
- Case managers, social workers, foster parents, case supervisors, program staff, program managers, program directors, quality assurance
Courses in this Series
SOGIE 101
Monday, May 23 from 1-4 p.m. ET
Inclusive Data Collection: How to Ask About SOGIE In Systems of Care
Tuesday, May 24 from 1-4 p.m. ET
Family Support with LGBTQ Children
Wednesday, May 25 from 1-4 p.m. ET
Gender Affirming Care
Thursday, May 26 from 1-4 p.m. ET
About the Training Series
Ruth Ellis Institute has developed the following training content through researching how adult practitioners, government health and human service employees, and staff at community-based organizations leverage their existing experience to integrate more affirming practices for lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth.
The development of this curriculum is embedded within a LGBTQ-specific direct service organization, ensuring that on-the-ground implementation is informing training content. Ruth Ellis’ model connects:
- Youth and their families lived experience
- Direct practice
- Research and evaluation
- Coaching and consulting
- Policy and regulations
Content in SOGIE 101 has been developed under two internal review boards, Wayne State University (2015-2017), and Michigan Department of Health and Human Services (2018-2021). The Ruth Ellis Institute surveyed over 600 participants through a pre-test, post-test, and three-month follow up to measure SOGIE knowledge, attitudes, and behaviors. The curriculum features content where there were statistically significant changes in participants outcomes regarding increases in support toward LGBTQ youth. These two courses are recommended for professionals who have not previously attended a SOGIE and/or LGBTQ youth training.
Trainers
Angelika Lewis (she/her/hers)
Education and Evaluation Coordinator
Ruth Ellis Center
Jessie Fullenkamp (she/her/hers), LMSW
Education and Evaluation Director
Ruth Ellis Center
Related Events
After repeated warnings from the Treasury Department that the federal government could run out of money and default on its debts as soon as June 1, lawmakers are scrambling to come up with a deal to keep the government solvent. In exchange for raising the debt ceiling, Speaker of the House Kevin McCarthy (R-Calif.) and the House GOP caucus insist the president agree to spending cuts for fiscal year 2024 – a non-starter, according to the president. However, given the prospect of a default, top staffers of McCarthy and President Joe Biden are working around the clock to come up with a compromise, with both sides hinting progress has been made. The outline of a potential deal revolves around the following issues:
An agreement on top-line spending numbers for fiscal year 2024 must be reached; however, members of both parties are opposed to decreasing portions of the discretionary budget, including military, environmental, and health care spending. Unspent funds of approximately $56 billion, according to the Congressional Budget Office, from previous COVID-19 packages are on the table for clawbacks, risking money already allocated to economic assistance. While Biden says he will not consider any changes to Medicaid access, McCarthy is pushing to include new work requirements for benefits programs, including Medicaid, food stamps, and TANF. Finally, members of both parties support reform to the permitting process for energy and other projects, but disagreements remain over the details.
President Biden cut his trip to Japan for the G7 meeting short so he could be back in Washington, D.C. to finalize the deal early this week.
HHS Reveals New Website to Find Mental Health Resources
The Department of Health and Human Services (HHS) launched a new website, FindSupport.gov, to help the public find resources and treatment for challenges related to mental health, drugs, or alcohol. The website offers visitors information on coping strategies, types of treatment, ways to help others, and payment options for treatment. The Substance Abuse and Mental Health Services Administration and the Centers for Medicare and Medicaid Services partnered to create the website after research showed the public sought a reliable and objective resource for dealing with mental health and substance use issues. Over the course of the project, HHS engaged 50 subject matter experts and collected feedback from people of all races, ethnicities, genders, education levels, and ages. FindSupport.gov is another national resource in addition to SAMHSA’s national helpline, 1-800-662-HELP, and the 988 Suicide and Crisis Lifeline. According to SAMHSA, almost one in three adults suffer from mental health and/or substance use isues.
New Fact from HHS on the End of the Public Health Emergency
To mark the end of the public health emergency (PHE) on May 11, 2023, the Department of Health and Human Services (HHS) released a new fact sheet called “End of the COVID-19 Public Health Emergency,” which details what will stay the same and changes to occur after over three years of the COVID-19 pandemic. In the fact sheet, the administration touted its accomplishments: 270 million people who received at least one dose of the vaccine as well as 750 million free COVID-19 tests, among other things. Since Jan. 2021, COVID-19 deaths are down by 95 percent and hospitalizations have decreased by 91 percent. With the end of the PHE, HHS says certain factors will remain the same, including telehealth flexibilities under Medicare through Dec. 2024 and indefinitely under Medicaid. However, Medicare and Medicaid will no longer have some of the other major flexibilities implemented during the pandemic. Certain waivers that expanded access and facility capacity, for example, will be halted. Moreover, the requirement of private insurance companies to cover COVID-19 testing without cost sharing ended on May 11.
New Low-Income Housing Bill Gains Bipartisan, Bicameral Support
On May 11, the Affordable Housing Credit Improvement Act made a comeback in the House of Representatives and the Senate with bipartisan support. Reps. Darin LaHood (R-Ill.), Suzan DelBene (D-Wash.), Don Beyer (D-Va.), Brad Wenstrup (R-Ohio), Jimmy Panetta (D-Calif.), and Claudia Tenney (R-N.Y.), along with Sens. Maria Cantwell (D-Wash.), Ron Wyden (D-Ore.), Todd Young (R-Ind.), and Marsha Blackburn (R-Tenn.) introduced the bill, which would increase the Low-Income Housing Tax Credit, an important tool for incentivizing private investment in the construction and renovation of affordable housing. The Affordable Housing Credit Improvement Act would increase the available credits by 50 percent, spurring the construction of 1.94 million additional affordable homes over the next ten years. It would also create almost three million jobs, increase tax revenue by $115 billion and support $333 billion in wages and business income. The bill would also incorporate stronger protections for veterans, victims of domestic and dating violence, as well as other underserved communities into the Low-Income Housing Tax Credit.
Subscribe to the Policy and Advocacy Radar to receive our biweekly policy roundup, which includes commentary on issues in Social Current’s federal policy agenda, opportunities to take action, and curated news and opportunities.






